Click here for the audio guide.
Please click see the video for an overview of the clinical manisfestation of a severe Ankylosing Spondylitis. It tells of a journey of the “Folded Man” and on his road to recovery.

ANKYLOSING SPONDYLITIS (AS)
- Also known as BECHTEREW’S DSE, MARIE STRUMPELL’S DSE, RHEUMATIOD SPONDYLOLITIS
- Prototype of seronegative spondyloarthropathies
Incidence:
- More common in males (3:1 ratio); more symptomatic and severely affected
- Female patients: have more peripheral joint involvement
- Age group: 20-40 yrs old
Clinical features:

- Sacroiliitis– hallmark of the disease
- Onset is insidious
- Presents a sharp, jolting pain in the buttock or hips
- Involves ligamentous insertion (enthesopathy), fibrocartilage and IV disc
Difference between mechanical causes of spinal disease and AS:
- Insidious onset
- Onset <40 yrs old
- More or less persistent discomfort for weeks to months
- Associated with morning stiffness
- Improvement with exercise (worse at rest)
- Diffuse radiation of pain to thoracic region and buttocks
- Asymmetrical decrease in ROM
- (+) Hip joint involvement
- (-) Neurologic deficit and (-) low back maneuver
- Involvement of other systems
- Peripheral joint involvement
- Typical extraspinal sites include:
- Manubriosternal joint
- Symphysis pubis
- Shoulder
- Hip joints
- Cardiovascular involvement
- Aortitis
- Fibrosis extending to mitral valve, septum or AV node
- Pericarditis
- Aortic insufficiency
- Left ventricular hypertrophy
- Anterior Uveitis
- Lung involvement
- Neurologic Problems
- Immune Neuropathy or Renal Amyloidosis (rare)
Diagnosis:
- Radiologic Examination
NEW YORK CLASSIFICATION of PELVIC X-RAYS
- 1 – blurring of joint margin
- 2 – narrowing of joint space
- 3 – erosions
- 4 – fusion
- Bamboo spine Deformity – syndesmophyte formation
- Patients may have inflammation of disk with destruction of adjacent vertebral bodies that radiographically resembles infection or tuberculosis (Romulus Lesions)
- Laboratory Findings
- No characteristic auto antibodies or immune abnormalities
- Nonspecific increase in ESR, anemia, increase in alpha 2 globulin
- Minority of patients are HLA-B27 positive especially if axial distribution is present
Treatment:
- NSAID (Indomethacin)
- Exercises
- Hydrotherapy
- Total hip replacement
Wedge osteotomy
PSORIATIC ARTHRITIS
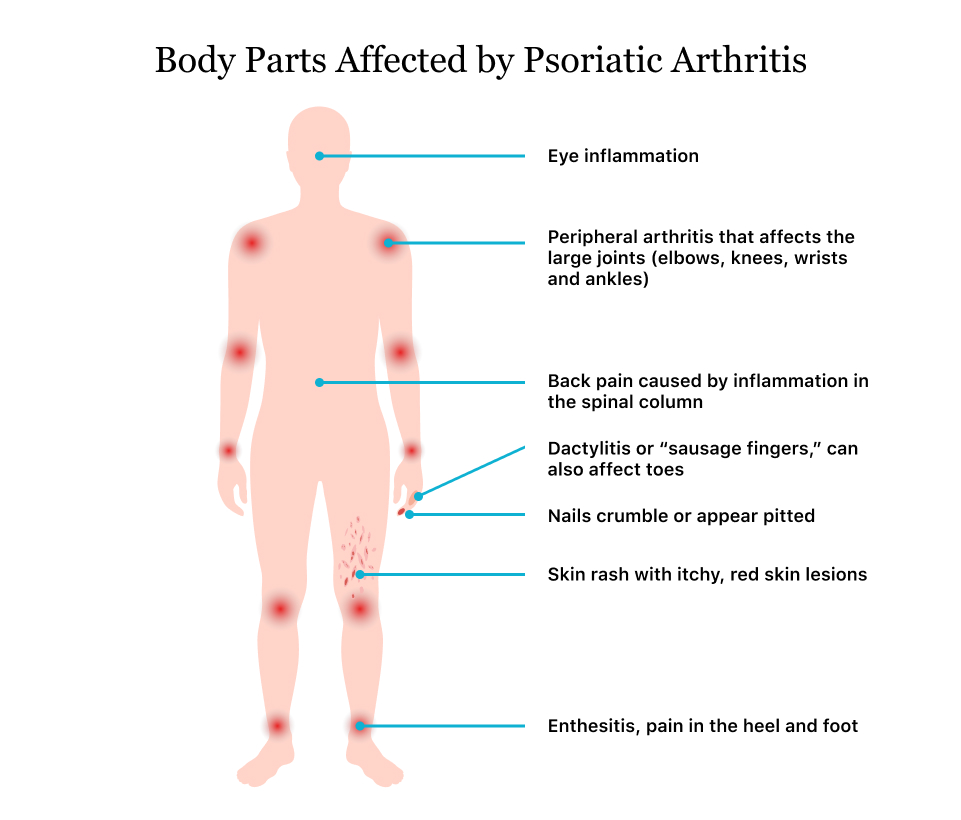
- Psoriasis is a benign inflammatory skin disease with genetic predisposition. Skin erosions are described as silvery scales most commonly located over the knee, elbows and scalp. Nail findings include stippling (pitting) and onycholysis.

Incidence:
- Male and female patients equally affected
- Onset is between 30-50 yrs old
Clinical Features:
- Gradual onset with skin disease often preceding a joint disease by months or years
- Auspitz sign

- Koebner response

- Sausage digits

- Enthesopathy
- Arthritis mutilans
- Opera glass hands

- Asymmetrical involvement; involves the UE earlier than the LE with joint stiffness of at least 30 mins
- Axial involvement of the SI joint is common
- Symmetrical involvement includes eye inflammation as conjunctivitis iritis, episcleritis and keratoconjunctivitis
General symptoms of PsA include:
- swollen, tender joints on one or both sides of your body
- morning stiffness
- swollen fingers and toes
- painful muscles and tendons
- scaly skin patches, which may get worse when joint pain flares up
- flaky scalp
- fatigue
- nail pitting
- separation of your nail from the nail bed
- eye redness
- eye pain
Laboratory Features:
- Radiographic Findings:
- Pencil point in cup deformity – whittling due to destruction of phalanges adjacent to the inflamed joints; seen in the end stage of the dse.
- Laboratory findings
- No characteristic auto antibodies or immune abnormalities
- Nonspecific; increase in ESR, anemia, increase in alpha 2 globulin
- Minority of patients are HLA-B27 positive esp. if axial distribution is present
Treatment:
- Skin measures
- NSAIDs / aspirin
- Sulfasalazine is effective for joint manifestation but no effect on cutaneous psoriasis
REITER’S SYNDROME

- A clinical triad of non-gonoccocal arthritis, conjunctivitis and urethritis
- Believed to be triggered by infection of the genitourinary tract caused by Clamydia, Campylobacter, Salmonella, Shigella and Yersinia
Incidence:
- Occurs mainly in young adult males
- If it occurs in females, HLA-B27 positivity is 100%
Clinical Features:
- Urethritis
- Discharge is mucopurulent,
- Prostatitis is common and in rare cases, hemorrhagic cystitis may be present
- Generally urine culture is negative but 20-40% have anticlamydial antibodies
- Conjunctivitis and iritis
- Usually bilateral (in contrast to anterior uveitis of AS)
- Arthritis
- Typically begins with weight bearing joints but is not symmetric
- Most commonly affected: knees, feet and wrist; arthritis of hands and fingers may give a sausage digit appearance
- Asymmetric small joint involvement esp. of the feet is more common in Reiter’s syndrome than AS
- Skin involvement
- Keratoderma blenorrhagica
- Balanitis Circinata
Laboratory Features
- Laboratory findings
- Elevated ESR and C-reactive protein
- Sterile pyuria
- Synovial fluid is purulent
- HLA-B27 is present in patients with axial dse
- Radiographic feature
- Erosions (after 2 mos resembling RA),
- Periosteal proliferation (in calcaneous, knees, and metatarsal bones)
Treatment
- NSAIDs such as indomethacin
- Acute stages:
- Bed rest and splinting
- ROM exercises
- Isometric strengthening exercises (started once swelling has subsided)
- Methotrexate or Azathioprine – given to patients with unremitting Reiter’s syndrome
- Antibiotics (Tetracycline) – given for treatment of urethritis & other extra –articular symptoms
- Intra-articular steroid – not recommended for long term therapy
TABLE 1 – COMMON SPONDYLOARTHROPATHIES
| Characteristics | Ankylosing Spondylitis | Reiter’s Syndrome | Psoriatic Arthritis | Enteropathic Arthropathy |
| Age of Onset | <40 yrs old | Middle aged adult | Young to middle age | Young to middle age |
| Onset | Gradual | Acute | Variable | Gradual |
| Sex | Male | Male | Equal | Equal |
| Sacroilitis or Spondylitis | 100% | <50% | 20% | <20% |
| Symmetry of Sacroiliitis | Symmetric | Asymmetric | Symmetric | Symmetric |
| Peripheral joint involvement | 25% | 90% | 95% | Frequent |
| Eye involvement | 25%-30% | Common | Occasional | Occasional |
| Cardiac involvement | 1-4% | 5-10% | Rare | Rare |
| Skin or nail involvement | – | Common | 100% | Uncommon |
| Triggered by infection | Unknown | Yes | Unknown | Unknown |
PRINCIPLES OF REHABILITATION INTERVENTION:
1. Rest
- Local Rest
- Systemic Rest
- Short Rest Periods
2. Exercise
- Passive Exercise
- Active Exercise
- Stretching Ex.
- Strengthening Ex.
- Endurance Ex.
- Aquatic Therapy
- Others
3. Treatment with Heat & Cold Modalities
4. Orthotic Devices
5. Assistive Devices & Adaptive Aids
6. Self-care
7. Patient Education
ENERGY CONSERVATION MEASURES
- Maximize biomechanical function of joints thru use of proper orthotics & assistive devices to effect energy-efficient ambulation & hand function
- Use appropriate adaptive devices & clothing
- Provide proper environmental design
- Have rest periods throughout the day
- Maintain ROM & strength
- Maintain proper posture
PRINCIPLES OF JOINT PROTECTION:
- Preservation of muscle strength and joint ROM and good joint alignment
- Prevention of positions of deformity especially in the hands.
- Utilization of the strongest joints (bigger joints) for the heavier jobs.
- Use each joint in its most stable anatomic and functional plane.
- Maintain muscle balance and correct patterns of motion.
- Adaptation of tasks requiring static positioning. It is best to alternate rest with activities.
- Elimination of activities that cannot be halted immediately.
- Application of scientific management principles to each task. Scientific management embodies work simplification and time and motion economy. Plan ahead and do not overdo nor underdo too much.
- Respect pain and stop activities that cause it.
- Provide support for inflamed joints.
- Use appropriate adaptive equipments & splints when necessary.
INFLAMMATORY BOWEL DISEASE
nflammatory bowel disease (IBD) is an umbrella term used to describe disorders that involve chronic inflammation of your digestive tract. Types of IBD include:
- Ulcerative colitis. This condition involves inflammation and sores (ulcers) along the superficial lining of your large intestine (colon) and rectum.
- Crohn’s disease. This type of IBD is characterized by inflammation of the lining of your digestive tract, which often can involve the deeper layers of the digestive tract.
Symptoms
Inflammatory bowel disease symptoms vary, depending on the severity of inflammation and where it occurs. Symptoms may range from mild to severe. You are likely to have periods of active illness followed by periods of remission.
Signs and symptoms that are common to both Crohn’s disease and ulcerative colitis include:
- Diarrhea
- Fatigue
- Abdominal pain and cramping
- Blood in your stool
- Reduced appetite
- Unintended weight loss
Causes
The exact cause of inflammatory bowel disease remains unknown. Previously, diet and stress were suspected, but now doctors know that these factors may aggravate but aren’t the cause of IBD.
One possible cause is an immune system malfunction. When your immune system tries to fight off an invading virus or bacterium, an abnormal immune response causes the immune system to attack the cells in the digestive tract, too. Heredity alsoseems to play a role in that IBD is more common in people who have family members with the disease. However, most people with IBD don’t have this family history.
Risk factors
- Age. Most people who develop IBD are diagnosed before they’re 30 years old. But some people don’t develop the disease until their 50s or 60s.
- Race or ethnicity. Although whites have the highest risk of the disease, it can occur in any race.
- Family history. You’re at higher risk if you have a close relative — such as a parent, sibling or child — with the disease.
- Cigarette smoking. Cigarette smoking is the most important controllable risk factor for developing Crohn’s disease.Smoking may help prevent ulcerative colitis. However, its harm to overall health outweighs any benefit, and quitting smoking can improve the general health of your digestive tract, as well as provide many other health benefits.
- Nonsteroidal anti-inflammatory medications. These include ibuprofen (Advil, Motrin IB, others), naproxen sodium (Aleve), diclofenac sodium and others. These medications may increase the risk of developing IBD or worsen the disease in people who have IBD.
Complications
Ulcerative colitis and Crohn’s disease have some complications in common and others that are specific to each condition. Complications found in both conditions may include:
- Colon cancer. Having ulcerative colitis or Crohn’s disease that affects most of your colon can increase your risk of colon cancer. Screening for cancer begins usually about eight to 10 years after the diagnosis is made. Ask your doctor when and how frequently you need to have this test done.
- Skin, eye and joint inflammation. Certain disorders, including arthritis, skin lesions and eye inflammation (uveitis), may occur during IBD flare-ups.
- Medication side effects. Certain medications for IBD are associated with a small risk of developing certain cancers. Corticosteroids can be associated with a risk of osteoporosis, high blood pressure and other conditions.
- Primary sclerosing cholangitis. In this condition, inflammation causes scarring within the bile ducts, eventually making them narrow and gradually causing liver damage.
- Blood clots. IBD increases the risk of blood clots in veins and arteries.
Complications of Crohn’s disease may include:
- Bowel obstruction. Crohn’s disease affects the full thickness of the intestinal wall. Over time, parts of the bowel can thicken and narrow, which may block the flow of digestive contents. You may require surgery to remove the diseased portion of your bowel.
- Malnutrition. Diarrhea, abdominal pain and cramping may make it difficult for you to eat or for your intestine to absorb enough nutrients to keep you nourished. It’s also common to develop anemia due to low iron or vitamin B-12 caused by the disease.
- Fistulas. Sometimes inflammation can extend completely through the intestinal wall, creating a fistula — an abnormal connection between different body parts. Fistulas near or around the anal area (perianal) are the most common kind. In some cases, a fistula may become infected and form an abscess.
- Anal fissure. This is a small tear in the tissue that lines the anus or in the skin around the anus where infections can occur. It’s often associated with painful bowel movements and may lead to a perianal fistula.
Complications of ulcerative colitis may include:
- Toxic megacolon. Ulcerative colitis may cause the colon to rapidly widen and swell, a serious condition known as toxic megacolon.
- A hole in the colon (perforated colon). A perforated colon most commonly is caused by toxic megacolon, but it may also occur on its own.
- Severe dehydration. Excessive diarrhea can result in dehydration.
IBD-associated arthritis is used to describe types of inflammatory arthritis associated with IBD and include psoriatic arthritis, ankylosing spondylitis and reactive arthritis.
PASQUIN, KYSSIE ANNE
RABANILLO, KATE ASELLE
SAGLAYAN, MADILEN KAYE
YBANEZ, KARINA MAY
1. How important is the role of Physical Therapy in the treatment of Ankylosing Spondylitis?
Ankylosing spondylitis presents decreased spinal mobility, decreased chest expansion, and tenderness of sacroiliac joints with direct pressure and with maneuvers that stress on joints. Symptoms first present morning stiffness and dull ache in the low backs or buttocks which usually begin in the late teens or 20s and is more common in males. Physical therapy plays a significant role in this condition since the initial treatment includes exercises that promote spinal extension that is usually facilitated by physical therapists. There are existing evidences about how exercise promotes mobility, improves function, and prevents severe deformity in many cases. According to Dr. Clegg in an article about how physical therapy helps ankylosing spondylitis, physical therapy for range of motion and posture are really important because if you are not in a good posture and have the unfortunate outcome of fusing in that position, that can be even more debilitating. In this case, physical therapy can also help with other symptoms including tendon pain and stiffness, and painful joints. With the help of physical therapy, correction of habits of movement and positioning in the early stage of ankylosing spondylitis may help maintain long-term mobility.
2. If you are given the time and resources to conduct a study or further research on the treatment of rheumatologic conditions, which condition should you give attention to?
Rheumatoid arthritis is a chronic autoimmune systemic inflammatory disease with unknown etiology. It has its peak age between 35 to 50 years and 2 to 3 times more common in women. It is incurable, progressive and affects the individual with 70% difficulty performing tasks, 33% cannot work after 5 years and have substantial disability after 10 years. There is no cure for RA, but there are non-pharmacological (exercises) and pharmacological medications recommended by your doctor which depends on your symptoms and duration of the said condition. The NSAIDs with the adverse effects (stomach irritation, heart problems, kidney damage), steroids (thinning of bones weight gain, diabetes), DMARDs (liver damage, bone marrow suppression, severe lung infections and lastly, a newer class of DMARDs, the biological agents (increases risk of infection).
In relation to the brief information provided regarding the rheumatoid condition and the adverse effects of its pharmacological medications, we would like to conduct a study which will deeply tackle the condition and will help in the development of drugs that will totally address the physiologic aspects of its causes and will not just delay the progression. Given the time and resources, we would like to come with a drug that will have less or possibly no serious adverse effects in order to fully provide comfort to the patients. Lastly, by developing this type of medication, the chance of increasing the numbers of recovery will be higher thus this condition will be addressed as curable.
3. Submit a question/s for discussion tomorrow regarding the topics posted.
Ankylosing Spondylitis: What should be the criteria for surgery to happen?
Psoriatic arthritis: What are the usual risk factors specifically for psoriatic arthritis?
Reiter’s Syndrome: Why do some people develop reactive arthritis in response to certain infections?
Irritable Bowel Movement: What is advisable to do first when you have irritable bowel movement? The home remedies like proper diet and exercises or to take pharmacological medications?
References:
Braddom, R. L. (2011). Physical medicine and rehabilitation, 4th ed. Elsevier Saunders. Philadelphia.
Vann, M. R. (2014). How physical therapy helps ankylosing spondylitis. Retrieved from: https://www.everydayhealth.com/conditions/how-physical-therapy-helps-ankylosing-spondylitis/
Zanni, G. R., PhD. (2010). Rheumatoid arthritis and women: a debilitating condition. Retrieved from: https://www.pharmacytimes.com/publications/issue/2010/february2010/featurera-0210
Rheumatoid arthritis. Retrieved from: http://mayoclinic.org/diseases-conditions/rheumatoid-arthritis/diagnosis-treatment/drc-20353653
LikeLike
Gayoso, John Louie
Lim, Jhia
Lima, Katrina Libertad
Olvido, Keana Alexa
1. How important is the role of Physical Therapy in the treatment of Ankylosing Spondylitis
People with Ankylosing spondylitis suffer with stiffness of the spine and other large joints in the body. The stiffness causes pain and decreases the ability to do tasks. With the help of physical therapy a person can improve their posture with proper alignment taught by a PT, pain management techniques such as hot packs and electric modalities and even strengthening exercises to improve endurance to be able to move more. A patient with Ankylosing spondylitis can manage to do more everyday tasks and improve their quality of life with the help of proper physical therapy treatment. Without physical therapy, they would just be relying on medication that can cause side effects and even harm their organs when taken excessively.
2. If you are given the time and resources to conduct a study or further research on the treatment of Rheumatologic conditions, which condition should you give attention to. (This includes all the ORS2 topics)
Given the opportunity, with enough time and resources, our group would like to pursue a research about the treatment for Juvenile Idiopathic Arthritis. Medications for this disorder only addresses or manages the symptoms such as to stop or slow down inflammation, but does not directly cure the root cause. Medications for this systemic disorder will give children a better prognosis and at the same time a shot at having a quality life ahead of them.
3. Submit a question/s for discussion tomorrow regarding the topics posted, Akylosing Spondylitis, Psoriatic arthritis, Reiter’s Syndrome and Irritable Bowel Syndrome. Questions submitted here will be our guide for tomorrow’s synchronous lecture.
1. What is the Hallmark of Ankylosing Spondylitis that differentiates it from other diseases?
2. What are the skin lesions or dermatological symptoms present in Reiter’s syndrome?
3. What differentiates Irritable Bowel Syndrome from Inflammatory Bowel Disease?
4. As physical therapists, what is our role in patients with Psoriatic Arthritis?
LikeLike
Javier, Esania Adrienne
Macavinta, Danica Rose
Maquiling, Yessamyr Johann
How important is the role of Physical Therapy in the treatment of Ankylosing Spondylitis?
Ankylosing Spondylitis also known as Bechterew disease, Marie Strumpell’s disease, and Rheumatoid Spondylolitis is a rare type of arthritic condition that causes stiffness and pain along the spine. This commonly starts in the lower back and spreads up to the neck and can damage joints in other parts of the body. The role of Physical Therapy in treating Ankylosing Spondylitis is very important because we help patients improve their joint mobility, posture, help them deal with pain, and help them with their ADL’s.
We subjectively give our patients specific exercises, activities, and training that fits the needs of each patient diagnosed with this condition. Exercises such as deep-breathing exercises, posture training, stretching, flexibility, strengthening exercises can help strengthen their muscles, improve their postures, joint mobility, decrease stiffness, and pain. We teach pain management techniques with the use of ice or heat packs to manage inflammation and pain in the joints. Another pain alleviating method is performing TENS (transcutaneous electrical nerve stimulation) to the patient.
Furthermore, we give them individualized activities to improve their functional ability and energy and help them reduce tiredness and fatigue. We also teach our patients to move their body efficiently when performing daily activities to avoid strains and other complications. In addition, we prescribe our patients to use assistive devices if needed, to improve their walking, to lessen their pain, and lessen their risk of falling and injuries. Lastly, we help our patients after surgery if advised by their doctor or physician.
If you are given the time and resources to conduct a study or further research on the condition, which condition should you give attention to?
My Mom currently suffers from Rheumatoid Arthritis. I have seen how painful it can get and there are times that no amount of pain relievers could relieve the pain she’s feeling. She does have her maintenance, goes to a rehabilitation center once in a while, and has her paraffin wax treatment here at home yet the pain is always there especially during night times. One of the major downsides of having RA is that it has no cure, the medications given to the patients are only to alleviate the pain as well as delay the deformities and effects of RA. Therefore, if I was given the time and resources to conduct a study or further research on a condition it would be Rheumatoid Arthritis. I want to be able to help in finding ways how RA can be stopped at an early stage of detection, and if possible, a cure.
Submit a question/s for discussion tomorrow regarding the topics posted, Akylosing Spondylitis, Psoriatic arthritis, Reiter’s Syndrome and Irritable Bowel Syndrome. Questions submitted here will be our guide for tomorrow’s synchronous lecture.
Questions:
General questions:
~What is the hallmark of each disease/syndrome?
~What is the gold standard for treatment of each disease/syndrome?
Inflammatory Bowel Disease
~What are the similarities and differences of Crohn Disease and Ulcerative Colitis?
~How is IBD different from irritable bowel syndrome (IBS)?
Ankylosing Spondylitis
~What does ankylosing spondylitis have in common with psoriasis and Crohn’s disease? How are they associated?
~What other disease or condition commonly accompanies ankylosing spondylitis?
Reiter’s Syndrome
~How is Reiter’s syndrome associated with reactive arthritis?
~Can sexual activity transmit this disease?
Psoriatic Arthritis
~Why do some people with psoriasis develop Psoriatic Arthritis?
~How can we prevent psoriasis and Psoriatic Arthritis flare-ups?
References:
APTA. (2020). Physical Therapy Guide to Ankylosing Spondylitis. ChoosePT. Retrieved from https://www.choosept.com/symptomsconditionsdetail/physical-therapy-guide-to-ankylosing-spondylitis#:~:text=Physical%20therapy%20will%20help%20improve,avoid%20slouching%20or%20forward%20bending.
WebMD. (2020). What Is Ankylosing Spondylitis?. Retrieved from https://www.webmd.com/arthritis/what-is-ankylosing-spondylitis#:~:text=Ankylosing%20spondylitis%20(AS)%20is%20a,other%20parts%20of%20your%20body.
LikeLike
JACOBO – MALHABOUR – MANA-AY – SAYSON
1. This condition is a rare type of arthritis results to pain and stiffness of the patient’s spine. One of the goals of physical therapy in this condition is to address the patient’s pain and discomfort improve the quality of the patient’s life. Another goal is to improve the patient’s posture since this condition affects the spine. Also, physical therapy aims to improve the range of motion of the patient. Keeping the patient active by formulating interventions that will cater ROM and posture can actually alleviate the pain experienced by the patient and as well as other symptoms. Lastly, what we think is one of the important roles of physical therapy in Ankylosing Spondylitis is patient education. Once we promote patient awareness and letting them know the importance of the interventions given, this will improve their performance, participation, and as well as their lifestyle. All of these will sum up to enable the patient to maintain their residual function to achieve the most functionality possible.
2. If you are given the time and resources to conduct a study or further research on the treatment of Rheumatologic conditions, which condition should you give attention to. (This includes all the ORS2 topics)
If given an opportunity to conduct a research for the treatment of any Rheumatologic conditions, our team would be focusing our research for the treatment of osteoarthritis. The reason for this is because osteoarthritis is the most common form of arthritis and a successful study in terms of its treatment would benefit a large population of patients that are suffering from an arthritic condition since it affect millions of people worldwide especially the elderly. Aside from its prevalence, OA is a debilitating condition because it commonly affect the hands and the large weight-bearing joints such as the knee and hip. In fact, OA is the most common musculoskeletal condition affecting these joints which are very important joints for function and basic ADL. And as a physical therapist our main goal is to help our patient function to their full potential and the prevalence and severity of osteoarthritis is what limits most of our patients especially those with arthritis to achieve these goals. Therefore, with the opportunity and enough resources our team would dedicate the time and effort to conduct a study to help our patients suffering osteoarthritis.
3.
Ankylosing Spondylitis
What are the specific exercises that should be performed in the rehabilitation of Ankylosing Spondylitis?
Is Ankylosing Spondylitis hereditary? How?
PSORIATIC ARTHRITIS
How does Psoriatic Arthritis progress? Does early diagnosis and intervention improve patient outcome?
Do lifestyle changes (diet or exercise) have an effect in the outcome of the treatment?
Reiter’s syndrome
Does Reiter’s syndrome affect the lifespan expectancy of the patient?
Is surgical intervention necessary for Reiter’s syndrome?
INFLAMMATORY BOWEL DISEASE
How long does the Inflammatory Bowel Disease last? Does it have a cure?
What are the PT interventions for Inflammatory Bowel Disease?
LikeLike
ALMOETE, Ma. Arjelyne
BEREBER, Marianne Jewel
DE LA TORRE, Ritcha Joy
EULA, Ianne Velle
1. How important is the role of Physical Therapy in the Treatment of Ankylosing Spondylitis
At the onset of AS, intermittent symptoms may occur affecting one side of the body. However, as it progresses, constant pain and stiffness become heightened. One of the most common symptoms of AS is low back pain and physical therapists play a big role in this aspect. The application of proper exercises, such as ROM, relieves the symptoms of AS which in turn can greatly benefit the patients with AS just by lessening the discomfort that they are feeling. Moreover, PTs also play a big role in patient education, this is to manage their disease effectively. PTs can evaluate patients with AS as patients show a flexed forward posture in clinical presentation. Finally, maintaining the function of the patient with AS is one of our top priorities. Aquatherapy can be a great help in reducing pain and symptoms along with breathing exercises and postural training, all of which Physical therapists play a huge part.
2. If you are given the time and resources to conduct a study or further research on the treatment of Rheumatologic conditions, which condition should you give attention to. (This includes all the ORS2 topics)
Further research on the treatment for Systemic Lupus Erythematosus is needed due to the following reasons: First, SLE has no cure yet, the discovery of new medications that will prevent organ damage and reduce the comorbidities can greatly save the lives of patients with SLE. Second, SLE is very common in women, there is an increased chance of miscarriage, due to a higher risk of complications like preeclampsia. With this, further study is needed to minimize the complications. Third, patients with SLE need immune cell-targeted therapy to eliminate the B cell expansion and function, a B-cell secrete autoantibodies that worsen the disease. We can further enhance this immune cell-targeted therapy for the rapid recovery of patients. Lastly, SLE management is very complex because there’s a variety of treatment options, especially in the area of medications, adverse-effect management, vaccination services, and pain management that increases the chance of SLE patient to develop secondary complications such as vasculitis, alopecia, mouth ulcerations, nephritis, pericarditis, peripheral neuropathy, cognitive impairment, anxiety, and depression. If given the time and resources, we can simplify the complexities of these treatments in order to lessen the burden of SLE patients especially if many organs are already involved.
3. Submit a question/s for discussion tomorrow regarding the topics posted, Ankylosing Spondylitis, Psoriatic arthritis, Reiter’s Syndrome, and Irritable Bowel Syndrome. Questions submitted here will be our guide for tomorrow’s synchronous lecture.
Ankylosing Spondylitis
1. How common is AS and who is most likely to get it?
2. How would you manage a patient with active Ankylosing Spondylitis with coexistent active multiple sclerosis?
Psoriatic Arthritis
3. What medication works best for psoriatic arthritis?
4. What aggravates psoriatic arthritis?
Reiter’s Syndrome/ Reactive Arthritis
5. How long does reactive arthritis take to develop?
6. Is reactive arthritis an STD?
Irritable Bowel Syndrome
7. What are the underlying mechanisms of IBS?
8. What foods should people with IBS avoid?
9. Problems in mental health are common in people with IBS?
10. Who is more likely to develop IBS? Men or women?
References:
Brent, L. (2020, September 23). Ankylosing Spondylitis and Undifferentiated Spondyloarthropathy Treatment & Management. https://emedicine.medscape.com/article/332945-treatment#d13
Toruner, C., and Diamond, B. (2012). Current and Novel Therapeutics in Treatment of SLE. Retrieved from: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3053574/#__ffn_sectitl
Sprigs, B. (2020). Systemic Lupus Erythematosus (SLE). Retrieved from: https://www.healthline.com/health/systemic-lupus-erythematosus#_noHeaderPrefixedContent
Manson, J. Rahman, A. (2006). Systemic lupus erythematosus. Retrieved from: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC1459118/#__ffn_sectitle
LikeLike
Balagosa, Maria Reyna
Bermudo, Ma. Kathrina
Gloriani, Nisa Marianne
Guion, Denise Sharielle
1. How important is the role of Physical Therapy in the treatment of Ankylosing Spondylitis?
– Physical Therapy has numerous benefits for people diagnosed with Ankylosing Spondylitis, it can be a valuable part of providing care. This includes components such as: stretching, improving posture, exercise, and modifications in the environment that would focus on the special needs of the patient for them to attain quality of life. Exercise is considered as a fundamental tool in managing AS together with pharmacological treatment. Postural assessment together with correcting misalignments is also a strategy that physical therapists utilize for people diagnosed with ankylosing spondylitis. Physical therapy can also help with symptoms such as: tendon pain and stiffness, and painful joints. In order to maintain long-term mobility and health, early interventions such as correcting habits of movement and positions are important factors in providing care. In addition, physical therapists create strategies or exercise plans that would work on developing or restore the mobility that was lost to the patient, improve movement of the spine, promote fitness, and decrease pain.
2. If you are given the time and resources to conduct a study or further research on the treatment of Rheumatologic conditions, which condition should you give attention to?
– As we discussed and thought about it thoroughly, we have selected Systemic Lupus Erythematosus as our topic of study. We have come to a conclusion that SLE should be given much more attention especially on how to treat it. SLE is a devastatingly deceptive disease, not only that but it is also debilitating and rapidly progressing. It has a broad spectrum of clinical manifestations and is rather hard to diagnose since most of the symptoms are similar to other conditions. SLE is usually managed by medical practitioners through the use of medications such as immunosuppressants in adjunct with physical therapy interventions.
As of the 21st century, SLE still has no cure. However, rheumatologists are trying to transition from prescribing broad immunosuppressants to more targeted treatment approaches. Thus, we would like to further research about combination therapies targeting several pathways and have an in depth knowledge about the immune system in order for us to have a medical breakthrough.
3. Submit a question/s for discussion tomorrow regarding the topics posted, Ankylosing Spondylitis, Psoriatic arthritis, Reiter’s Syndrome and Irritable Bowel Syndrome.
1. Miss I am quite confused with the notion that Sun exposure can trigger psoriasis but at the same time UV therapy is used to treat psoriasis.
2. Aside from radiologic examination can MRI be used as a diagnostic modality for Ankylosing Spondylitis?
3. Patients experience psoriatic arthritis and it becomes worse. Is it life threatening? Is this type of arthritis drug dependent? What if they cannot take the medication the symptoms will get worse? What are the PT managements in order to help patients with psoriatic arthritis?
4. Is this type of arthritis drug dependent? What if they cannot take the medication the symptoms will get worse?
5. What are the PT managements in order to help patients with psoriatic arthritis?
6. What is the difference between Irritable Bowel Syndrome from Inflammatory Bowel Disease?
Extra (fun) questions:
1. Who is your bias in BTS? Why and how?
2. Top 3 favorite songs of BTS.
References:
Friedlander, J. (2020). Ankylosing Spondylitis and Physical Therapy: Benefits, Exercises, and More. https://www.healthline.com/health/ankylosing-spondylitis/as-and-physical-therapy-benefits
Vann, M. (2014). How Physical Therapy Helps Ankylosing Spondylitis. https://www.everydayhealth.com/conditions/how-physical-therapy-helps-ankylosing-spondylitis/
Pullen, L.C. (2019). Lupus Treatments: Into the Future. https://www.the-rheumatologist.org/article/lupus-treatments-into-the-future/
Wickham, M.B.,& Felz. M. (2016). Systemic Lupus Erythematosus: The Devastatingly Deceptive Disease. https://www.mdedge.com/clinicianreviews/article/110888/immunology/systemic-lupus-erythematosus-devastatingly-deceptive/page/0/1
LikeLike
Group: DEOCAMPO’S group
Members:
-DEOCAMPO, Bryan Melvin
-CORDOVA Rachelle Andrea
-GENERAL, Ma. Jamille
-BELARMINO, Lian Marion
For ORS 2
1. How important is the role of Physical Therapy in the treatment of Ankylosing Spondylitis
– Ankylosing Spondylitis (also called Bechterew disease) an arthritic condition that mainly affects the spine of a person, with the affectation of this sensitive area Physical therapy plays a vital role in the restoration and wellness of the person. Physical therapy and every physical therapist in treating this condition are important in a way that they administer and conduct physical activities to possibly remediate and prevent progression of the condition and also through modifying the environment and functional method/ways of every patient. Ankylosing spondylitis (AS) causes pain, stiffness, and inflammation of the spine causing LOM, this limited movement of the spine or the overall limitation in normal motion of a person is treated by every PT through, strengthening exercises, ROM exercises, stretching exercises, cardiovascular training, and also AS causes postural disturbances so PT also conducts posture training in order to restore posture and prevent further malalignments in the patient. PT also educates the patient and his/her caregivers for the proper body mechanics in doing the usual activities or modifying the patient’s movements and the environment for safer execution and for preventing secondary complications. The bottom line Physical therapy is essential in patients with AS due to its good effects and favorable results such as restoring, maintaining, and improving functional capacity and mobility of the patient, and also alleviating pain and stiffness felt by patients with AS.
2. If you are given the time and resources to conduct a study or further research on the treatment of Rheumatologic conditions, which condition should you give attention to. (This includes all the ORS2 topics)
-If we as a group were given the time and resources to conduct a study or further research on the treatment of Rheumatologic conditions, conditions that we would give attention to are Arthritis and Osteoarthritis. We being students of physical therapy, our goal is to provide interventions to deal with conditions that negatively impact the patient’s capabilities to interact with the world and to improve the quality of life that they’re experiencing; to “give life to years” as what our teachers say. For RA and OA are conditions that are commonly seen in patients that we encounter in the clinical setting and which affects the joints, a part of the body that gives the patient a capability to move through an area of space and to interact with it; though both differ in their means in establishing their effects (RA being a condition that is caused by an abnormal autoimmune response while OA being a condition that is caused by a progressive destructive process) these conditions, at the end, cause negative effects to the patient’s joints. And with these reasons, it really shows its importance for us. As a summary, the reason why we picked these conditions is because it is 2 of the most commonly seen arthritic conditions in the clinical setting; that there are 2 of the most common diseases that causes the symptoms that pushe the patient to seek rehabilitative care.
3. Submit a question/s for discussion tomorrow regarding the topics posted, Akylosing Spondylitis, Psoriatic arthritis, Reiter’s Syndrome and Irritable Bowel Syndrome. Questions submitted here will be our guide for tomorrow’s synchronous lecture.
1st question: Does the spine bones inflammation or erosion of ankylosing spondylitis is similar to the inflammation of Juvenile Idiopathic inflammation specifically the pauciarticular classification and the enthesitis-related arthritis of JIA?
2nd question: Which is worst in terms of prognosis ankylosing spondylitis or Reiter’s syndrome?
Additional Ideas are taken:
APTA.(2020). Physical Therapy Guide to Ankylosing Spondylitis. https://www.choosept.com/symptomsconditionsdetail/physical-therapy-guide-to-ankylosing-spondylitis
Friedlander, J.(2020). Ankylosing Spondylitis and Physical Therapy: Benefits, Exercises, and More. https://www.healthline.com/health/ankylosing-spondylitis/as-and-physical-therapy-benefits#exercises
Dagfinrud H, Hagen KB, & Kvien TK.(2008). Physiotherapy for ankylosing spondylitis.https://www.cochrane.org/CD002822/MUSKEL_physiotherapy-for-ankylosing-spondylitis
LikeLike
Dela Llana, Lexie
Richardson, Blessy
Tenefrancia, Gilean
1. How important is the role of Physical Therapy in the treatment of Ankylosing Spondylitis
The primary role of every physical therapist is to aid the recovery of the patient’s physical health and achieve their optimum level of functioning. Patients with Ankylosing Spondylitis are likely to experience joint pains which would progressively cause the patient’s range of motion to decrease and would also cause alterations on the patient’s posture. The use of physical therapy skills to patient with AS can help reduce pain, increase mobility, prevent contractures, correct postural malalignment, and improve overall wellness through various exercises and education. . Physical therapy intervention includes aerobic training, stretching exercises, range of motion exercises, the use of pain reducing modalities, patient education, etc. According to a study by Moreno, et. al, patients with AS showed a favorable response with physical therapy promoting remission to the disease due to its anti-inflammatory and biomechanical effects. Additionally, a multimodal physical therapy program which includes aerobic, stretching, and pulmonary exercises in adjunct with routine medical management has shown greater improvements. Although pharmacologic therapy could provide much relief to the symptoms of AS, physical therapists still plays a vital role in managing the treatment of AS.
References:
Ankylosing Spondylitis. (2020, October 5). Physiopedia, . Retrieved 07:01, November 20, 2020 from https://www.physio-pedia.com/index.php?title=Ankylosing_Spondylitis&oldid=252717.
Vann, M. & Mercellin, L. (2014). How Physical Therapy Helps Ankylosing Spondylitis. Retrieved from https://www.everydayhealth.com/conditions/how-physical-therapy-helps-ankylosing-spondylitis/
Tricás-Moreno, J. M., Lucha-López, M. O., Lucha-López, A. C., Salavera-Bordás, C., & Vidal-Peracho, C. (2016). Optimizing physical therapy for ankylosing spondylitis: a case study in a young football player. Journal of physical therapy science, 28(4), 1392–1397. https://doi.org/10.1589/jpts.28.1392
Goodman, C. C., & Fuller, K. S. (2015). Pathology: Implications for the Physical Therapist. St. Louis, MO: Elsevier Saunders
2. If you are given the time and resources to conduct a study or further research on the treatment of Rheumatologic conditions, which condition should you give attention to. (This includes all the ORS2 topics)
If we were given the chance to conduct a research on one rheumatic condition, we would explore further on the treatment for the Polyarticular & Systemic-onset subclasses of the Juvenile Idiopathic Arthritis. They are associated to result in severe disability among other forms of JIA and their causes are still unknown (Goodman & Fuller, 2015). Although there are already established treatments to approach these conditions, we still want to aim to halt the disease progression and minimize the damage it causes to the patients. Since these diseases have an early-onset (childhood), it would totally affect the quality of life of the person at an early age, which would limit their activities as a child and affect their holistic growth. As much as possible we do not just want to research on treatments, but also preventions and early detection for susceptibility.
Reference
Goodman, C. C., & Fuller, K. S. (2015). Pathology: Implications for the Physical Therapist. St. Louis, MO: Elsevier Saunders
3. Submit a question/s for discussion tomorrow regarding the topics posted, Ankylosing Spondylitis, Psoriatic arthritis, Reiter’s Syndrome and Irritable Bowel Syndrome. Questions submitted here will be our guide for tomorrow’s synchronous lecture.
•What is the differential diagnosis bet ankylosing spondylitis and seropositive polyarticular aside from age?
•It was mentioned that psoriatic arthritis is a mild disease but can cause significant hand deformities. What are the specific PT treatments to maintain hand function despite affection of the fingers?
LikeLike
GROUP TAMBANILLO, TUBAR, AND TUGBANG
The T’s
3-B
1. How important is the role of Physical Therapy in the treatment of Ankylosing Spondylitis
Physical Therapy is important in treating Ankylosing Spondylitis because it involves training and exercises that may help the patient recover to his/her functional capabilities. Training or exercises may also improve the patient’s posture such as maintaining an upright posture, strengthen the muscles that may aid with the patient’s upright posture, increase the flexibility of the patient’s joints to prevent stiffness, improve the patient’s chest expansion and breathing, improve energy, and reduce fatigue.
2. If you are given the time and resources to conduct a study or further research on the treatment of Rheumatologic conditions, which condition should you give attention to. (This includes all the ORS2 topics)
We would like to consider the conditions: (1) Extended Oligoarthritis, (2) Enthesitis-Related Arthritis, and (3) Psoriatic Arthritis all because of the new treatment adjunct of Etanercept as a TNF-inhibitor. As of now it has completed it’s 8-year extended trial after completion of Phase III trials thereby it is considered safe and effective for this 3 condititions (Foeldvari et al., 2019, p. 21). Although as of this recent discovery we would like to highlight that the trials indicated that 50mg of Etanercept is being administered every week per participant and according to (Gronseth & Messé, 2016) that a 25mg injected Etanercept costs around $440.00 and that without mentioning costs of pretreatment evaluation and perispinal administration of the drug which may costs around $1,100.00 all in all. Thereby we do think that it is best that we need to further lengthen the horizon for other effective, safe, and ideally cost-effective nonpharmacologic treatments for these diseases.
Even more to mention that with that of price range of medication, how much more would individuals situated in 3rd world countries suffer for the efficacy of the drug. This is where Physical Therapy stands. Aside from pharmacotherapy as an adjunct to our interventions, with further research we may be able to come up with an a better answer/alternative for the treatment and management of patients suffering from these conditions.
3. Submit a question/s for discussion tomorrow regarding the topics posted, Akylosing Spondylitis, Psoriatic arthritis, Reiter’s Syndrome and Irritable Bowel Syndrome. Questions submitted here will be our guide for tomorrow’s synchronous lecture.
Ankylosing Spondylitis
– What is the role of genetics in AS?
– What are the possible radiographic findings to diagnose AS?
– What are the indications for surgery?
Psoriatic arthritis
– What is the role of genetics?
– Can stem cell therapy treat it?
– What is the role of Physical Therapy in Psoriatic arthritis?
Reiter’s Syndrome
– What are indications for surgery?
– What are the possible complications?
– Which skin and nail findings are characteristic of reactive arthritis?
Irritable Bowel Syndrome
– How is it usually managed?
– How are bowel habits altered with patients having this syndrome?
– What diets can reduce the symptoms of IBS?
REFERENCES:
-Physical Therapy Guide to Ankylosing Spondylitis.(2015).Retrieved at https://www.choosept.com/symptomsconditionsdetail/physical-therapy-guide-to-ankylosing-spondylitis#:~:text=Physical%20therapy%20will%20help%20improve,avoid%20slouching%20or%20forward%20bending.
-Gronseth, G. S., & Messé, S. R. (2016). Practice advisory: Etanercept for poststroke disability: Report of the Guideline Development, Dissemination, and Implementation Subcommittee of the American Academy of Neurology. Neurology, 86(23), 2208–2211. https://doi.org/10.1212/WNL.0000000000002735
-Foeldvari, I., Constantin, T., Vojinović, J., Horneff, G., Chasnyk, V., Dehoorne, J., Panaviene, V., Sušić, G., Stanevicha, V., Kobusinska, K., Zuber, Z., Dobrzyniecka, B., Nikishina, I., Bader-Meunier, B., Breda, L., Doležalová, P., Job-Deslandre, C., Rumba-Rozenfelde, I., Wulffraat, N., Pedersen, R. D., … Paediatric Rheumatology International Trials Organisation (PRINTO) (2019). Etanercept treatment for extended oligoarticular juvenile idiopathic arthritis, enthesitis-related arthritis, or psoriatic arthritis: 6-year efficacy and safety data from an open-label trial. Arthritis research & therapy, 21(1), 125. https://doi.org/10.1186/s13075-019-1916-9
LikeLike
ZARAGOZA AND SALCEDO, BSPT-3B
1. How important is the role of Physical Therapy in the Treatment of Ankylosing Spondylitis
The role of physical therapy in Ankylosing Spondylitis is vital. As part of our intervention, we could educate and exercise the patient to improve quality of life. We should educate our patients on what activities could alleviate this condition such as smoking, falls, and therefore prevent such activities. In addition, we could educate them on how to perform correct positions, and proper lifting techniques to avoid stress in their spine. Also, we could perform therapeutic intervention such as trunk range-of-motion and strengthening exercises to minimize thoracic kyphosis to prevent pulmonary complications, aerobic stretching for shortened muscle, pulmonary exercises, and chest expansion to improve spinal mobility, work capacity, encourage low-impact aerobic exercise with emphasis on extension and rotation. Lastly, we could do some aquatic exercises and relaxation techniques, energy conservation, and recommend tools or aids in order to maintain the posture in an optimal position. This education and intervention, greatly influence the patient’s ROM, mobility, and posture which leads to better outcomes and high quality of life. As physical therapists we all know that this type of condition is very serious that is why one of our main goals is to alleviate the pain in order to perform an effective intervention to the patients that have this condition. We also not just want to give intervention but also we want to check it’s functional capacity before conducting certain exercises.
2. If you are given the time and resources to conduct a study or further research on the treatment of Rheumatologic conditions, which condition should you give attention to. (This includes all the ORS2 topics)
Systemic Lupus Erythematosus is one of the conditions we are interested to study and research about. SLE a decade ago was one of the diseases that have a poor prognosis and many of its features were not known. However, as time goes by a lot of studies have arisen which deepened our knowledge of its mechanism up to molecular biology which leads to producing therapeutic management for this disease and leads the patients to better outcomes or prognosis. Despite all of this management, there is still no cure for this disease. SLE has life-threatening complications and it is worth it to give such attention and research. The possible causes of this disease are genetics, infection, UV rays, extreme stress, pregnancy, drug-induce, and smoking. As a researcher with enough time and resources, we could deeply study the genetic component, pharmacologic treatments, and utilize gene therapy for this condition. As physical therapists we always see geriatric patients suffer from this kind of condition and that is why we want to further research about this condition in order to contain this condition and can make people that have this condition live a normal life. Finding a cure for this disease is hard, and we are aware of that but for us, we know that all of the problems have a solution, and we know that there is a cure that’s just waiting there to be discovered.
3. Submit a question/s for discussion tomorrow regarding the topics posted, Ankylosing Spondylitis, Psoriatic arthritis, Reiter’s Syndrome, and Irritable Bowel Syndrome. Questions submitted here will be our guide for tomorrow’s synchronous lecture.
Miss, we have a question regarding the treatment of psoriasis arthritis, What if the patient will have an allergic reaction to NSAIDs?
Reference:
Guccione, A.A., Wong, R.A., Avers, A,(2012) Geriatric Physical Therapy. Missouri: Mosby, Inc.
LikeLike
Librella, Melfe (3A)
Malapit, Katherine (3B)
Subong, Ma. Nicole (3B)
1. Physical Therapy has a great role in treating Ankylosing Spondylitis (Dagfinrud, Hagen, & Kvien, 2008) because it maintains or improve movement of the spine, improve fitness and decrease pain. According to Tricás-Moreno J.M., et. al (2016), pain relief, normal joint mobility, improved muscle function, return to activities of daily living and competitive sporting activities were note to a football player who was given physical therapy treatment such as aerobic exercises, stretching and therapeutic exercises and thermotherapy.
References:
Dagfinrud, H., Hagen, K. B., & Kvien, T. K. (2008, January 23). Physiotherapy for ankylosing spondylitis. Cochrane.
https://www.cochrane.org/CD002822/MUSKEL_physiotherapy-for-ankylosing-spondylitis
Tricás-Moreno, J. M., Orosia Lucha-López, M., Carmen Lucha-López, A., Salavera-Bordás, C., & Vidal-Peracho, C. (2016).
Optimizing physical therapy for ankylosing spondylitis: a case study in a young football player. Journal of Physical Therapy Science, 28(4), 1392–1397. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4868250/
2. Polymyalgia Rheumatica has interestingly caught my attention from all the ORS2 topics. It is a systemic rheumatic inflammatory disorder with an unknown cause, I think it would be a nice topic for research due to the mystery of the unknown. Aside from this, Polymyalgia Rheumatica is a condition that commonly affects the axial areas like the neck, shoulder and pelvic girdle but also affects the temporal artery induced by giant cell arteritis. Furthermore, it can also affect the jaw that leads into misdiagnosis as temporomandibular joint disorder. In order to lessen the misdiagnosis a research in this topic is valuable in my opinion. Knowing and understanding the cause of PMR can help to distinctly differentiate it from TMJ or any other rheumatic disease with the same signs ang symptoms.
3. Q1: Why does ankylosing spondylitis have many other names? Was Bechterew or
Strumpell not aware that the disease is already named after the other?
Q2: Why is ankylosing spondylitis more common in males? Is it sex-linked?
Q3: Among those listed in the blog post, which is the Gold standard treatment for
ankylosing spondylitis?
Q4: Why are eye conditions (e.g. uveitis, conjunctivitis, and keratoconjunctivitis) commonly seen in
arthritic conditions?
Q5: Can Reiter’s syndrome be sexually transmitted?
LikeLike
Rodlyn Olete, Dezreel Alfuente, Renee Latade, Joselito Lorenzo
1. Physical Therapists play a significant role in treating Ankylosing Spondylitis. During PT, to alleviate pain and stiffness caused by Ankylosing Spondylitis, The patient can learn about various exercises you can do on a daily basis. Physical Therapists will help in improving posture and joint mobility to prevent slouching or forward bending. Flexibility exercises are also recommended to help maintain and improve joint mobility. Strengthening exercises given by PTs to their patients also play a role to help strengthen back and abdominal muscles to help maintain proper posture. Deep-breathing exercises also improve chest expansion and help the patient breathe better which can help with improving blood flow. Electrotherapy can also be used to alleviate pain. To conclude, PTs have a significant role in treating patients with Ankylosing Spondylitis in terms of managing pain, improving posture, and joint mobility to help the patient perform everyday activities in a more functional way,
2. Our group decided to choose PMR. Since it is a Systemic Rheumatic Inflammatory disorder, the affectation is worse as compared to other arthritic conditions. Furthermore, it can cause arterial rupture which can lead to stroke. The etiology of PMR is unknown since contributing factors are inconsistent. I think that if we are able to identify the major contributing factor, we are able to create awareness and prevention programs that can help lower the cases of this disease
3.
* Are there ways to lower your risk of having arthritic conditions ?
* Other than signs and symptoms given are there other manifestations to help early detection of arthritis
LikeLike
Conlu
Dimafiles
Dorde
Mecuando
1. Ankylosing Spondylitis (AS) is an arthritic condition affecting the spine. It causes pain and stiffness that usually starts at the lower back area. Currently, it has no known cure but therapy is one of the best managements for AS. Although there are medications, being active is a better way to remediate pain. This is why physical therapy is important because therapists can teach exercises to a patient with AS that can address the pain and tight muscles.
2. The disease that we would want to study on is rheumatoid arthritis, an autoimmune and idiopathic disease that a lot of people suffer from. Since it is idiopathic, we would like to know and understand more what triggers this disease, how to prevent it, and how to cure it.
3. Questions:
a. What are the proper ways to treat and care for psoriatic arthritis?
LikeLike
Kim Francis Balledos – 3A
Oliver Gonzales – 3A
Edmar Sumagaysay – 3B
1) How important is the role of Physical Therapy in the treatment of Ankylosing Spondylitis People with Ankylosing spondylitis suffer with stiffness of the spine and other large joints in the body.
Physical therapy can help deal with the stiffness and pain associated with the condition, with further improvement in the ability to do more tasks. The therapists can provide strengthening and movement exercises to allow the patient to improve his/her endurance so he/she can be able to move more. Without physical therapy, and with total reliance on medications alone, the deleterious effects would outweigh the beneficial effects it would supposedly provide. Total increase in the quality of life for patients with ankylosing spondylitis is a great benefit that comes with intensive physical therapy intervention.
2) If you are given the time and resources to conduct a study or further research on the treatment of Rheumatologic conditions, which condition should you give attention to. (This includes all the ORS2 topics)
If we were given an opportunity to conduct a study, we would primarily focus on finding an optimal approach towards diagnosing and treating patients with Polymyositis Rheumatica (PMR). The disease is a systematic rheumatic inflammatory disorder, it is also a disorder of unknown etiology. Since there are no definitive tests in order to identify PMR, it can be really difficult to interpret a disease that can lead to a severe disability. We do think that dwelling upon this disease can help unravel its unknown causes and further improve its diagnosis and management, which can be beneficial to patients, researchers, and healthcare practitioners in developing efficient and effective strategies to combat this disease.
3) Submit a question/s for discussion tomorrow regarding the topics posted, Akylosing Spondylitis, Psoriatic arthritis, Reiter’s Syndrome and Irritable Bowel Syndrome. Questions submitted here will be our guide for tomorrow’s synchronous lecture.
Q1: What neurotransmitter is imbalanced in IBS?
Q2: Where does chronic inflammation occur in ankylosing spondylitis?
Q3: What is the radiographic hallmark or psoriatic arthritis?
Q4: In Reiter syndrome, what are the triad of symptoms that marks the presence of the disease?
Reference:
Cbp, P. M. C. G. C., & Ncs, P. K. F. S. (2020). Goodman and Fuller’s Pathology: Implications for the Physical Therapist (5th ed.). Elsevier.
LikeLike